Service

Digital Non-mydriatic Fundus Camera
- Instant images of your retina to detect Diabetic Retinopathy
Diabetic Retinopathy is one of complications in which Retina of eye is affected in cases of Uncontrolled Sugars. Uncontrolled Sugars lead to formation of abnormal blood vessels which are more fragile in Retina which may give rise to bleeding in retina which inturn may cause permanent blindness. To prevent such permanent cause of Blindness Sugar levels should be controlled along with other Risk factors like Blood pressure and Cholesterol.
And as routine Annual Screening Of Retina to be done to know whether signs of Retinopathy has developed or not which could be tackled in early stages to prevent vision loss.Screening of Retinopathy can be done with Fundus Imaging Machine.If you have already developed Retinopathy then our Retina Specialist will help you in preventing further deterioration of Vision. Those who have developed Retinopathy will require Frequent Screening by Retina Specialist, frequency depends upon stage of Retinopathy. So prevention is better than treatment, hence annual Screening for every Diabetic patient is recommended.

Ankle Brachial Index/Toe Brachial Index
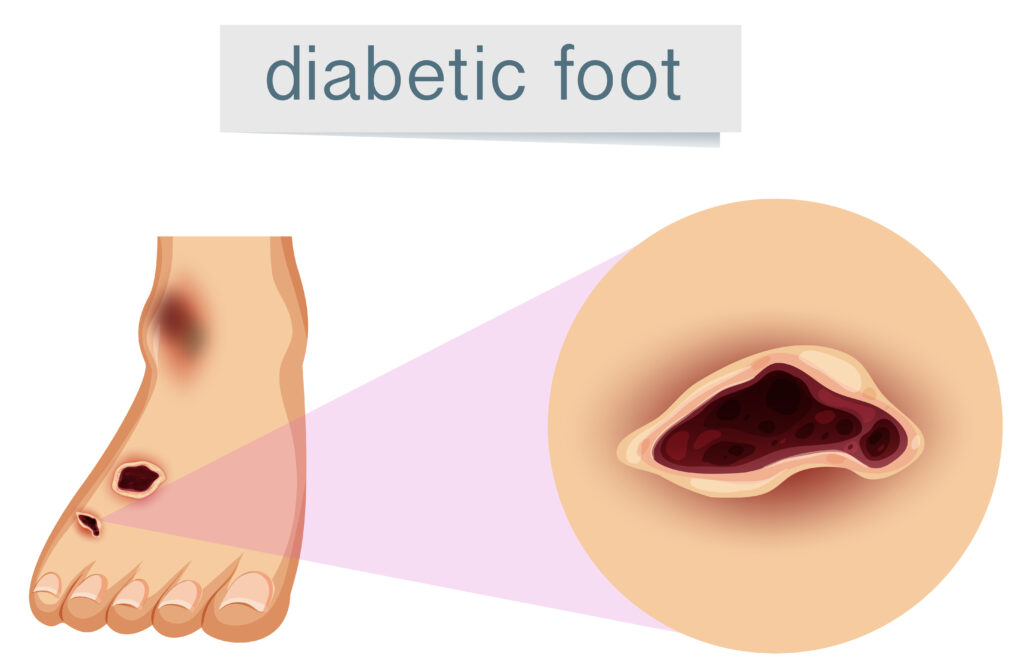
Uncontrolled Diabetes can lead to developing blockages in lower limb arteries, poor circulation can lead to Gangrene of lower limb if Vascular circulation is severely compromised. If ulcer has been developed in Uncontrolled Diabetes then it becomes difficult for ulcer to heal with compromised circulation of lower limbs. So for prevention of Amputation and to know vascular status of your lower limbs annual screening of Your vascular circulation of lower limbs is essential.


Neuropathy Assessment
- Quantitative Assessment of Diabetic Neuropathy
Uncontrolled Diabetes can affect nerves of lower limb which could lead to loss of Protective Sensation. Loss of protective sensation could lead to skin breakdown and ulcer formation which could subsequently leads to amputation. To prevent such complications Annual Screening for checking Quantitative Assessment of Diabetic Neuropathy is essential. By doing so we can offer treatment to such patients which essentially comprises of Good Sugar Control, and Control of Other risk factors like Hypertension and Cholesterol, Abstinence from Smoking and alcohol and providing then with corrective footwear to prevent further damage caused by Neuropathy.

Plantar Pressure Assessment
- Assess the risk of ulceration
- Offload the excess pressure
- Get apt footwear solutions
Uncontrolled Diabetes can affect nerves of lower limb which could lead to loss of Protective Sensation. Loss of protective sensation could lead to skin breakdown and ulcer formation which could subsequently leads to amputation. To prevent such complications Annual Screening for checking Quantitative Assessment of Diabetic Neuropathy is essential.


CGMs (Continuous Glucose Monitoring System)
- Type 1 Diabetics who are on multiple doses of insulin.
- Type 2 Diabetics who are on insulin as well on Oral Anti Diabetic Drugs to adjust the medication customized to one’S own eating pattern and carbohydrate intake. Dietary Modification and Medication adjustment becomes easy. Thus helping to adjust right medication and in right dose eventually resulting into much better sugar control.
- Gestational Diabetes Mellitus where multiple pricks can be avoided to measure blood sugar.
- Brittle Diabetes where Sugar Readings and HBAIC does not correlate.
It’s a method which measures your blood Glucose every 15 minutes for 14 days without repeated pricks. It involves painless insertion of sensor on your arm which measures and records Glucose readings every 15 minutes for 14 days. Information is reader through reader available with physician and interpreted by physician.
Who requires CGMs.
We at Dr .Nayaks Diabetic Clinic offer you CGMS with Customized Diet chart and appropriate medication adjustment which helps to reduce pill burden.

Orthotics ( Diabetes Footwear Specialist)
We at Dr Nayaks Diabetic Clinic care for your feet .Our Orthotic Specialist evaluate your feet requirement and make Customized Insoles or Footwear . Many of Diabetic have Unnoticed Foot deformities like Flat Feet, High Arch Feet, toe deformities which require thorough evaluation and identification of high pressure Zones in your feet which are high risk for ulceration. By doing so we are preventing your risk of getting ulcers and subsequent amputation. Many of feet pain can be vanished just with appropriate Footwear Modifications . So Orthotics plays very important role in your Feet care.


Diabetes Health Screening Package
- Complete Blood Count
- Renal Function test
- Liver Function Test
- Fasting Blood Sugar
- Post Lunch Blood Sugar
- HBAIC By HPLC Method
- Lipid Profile
- Thyroid Function Test
- Urine Alnumin/Creatinine Ratio
- EGFR
- Urine R/M
Above Package Includes Diabetes Related Kidney Involvement.
Hurry Up….Call Now
Podiatry (Diabetic Foot Care)
We pledge to save amputation of every Diabetic patient. Feet are unfortunately most neglected part in Diabetes. We as team of Dr Nayak’s Diabetic Clinic would help you to prevent Diabetic Foot Complications.
Diabetic foot care helps in preventing and managing foot complications amongst people with Diabetes.
Prevention can be done in simple manner as follows







Frequently Asked Questions
Type 2 diabetes is a genetic condition or pre-disposition that doesn’t change with treatment. But diabetes is defined as an elevated blood sugar.
When your blood sugar is normal with no treatment, then the diabetes is considered to have gone away. However, even when the blood sugars are controlled, because type 2 diabetes is a genetic condition, the predisposition for diabetes always exists. High blood sugars can come back.
If you have type 2 diabetes and the blood sugar is controlled during treatment (diet, exercise and medications), it means that the treatment plan is working. You are getting the good blood sugar because of the treatment – NOT because diabetes predisposition has gone away. You will need to continue your treatment; otherwise your blood sugar will go back up.
If you cannot normalize or control the blood sugars with diet, weight loss and exercise, the next treatment phase is taking medicine either orally or by injection.
Diabetes pills work in different ways – some lower insulin resistance, others slow the digestion of food or increase insulin levels in the blood stream. The non-insulin injected medications for type 2 diabetes have a complicated action but basically lower blood glucose after eating. Insulin therapy simply increases insulin in the circulation.
Don’t be surprised if you have to use multiple medications to control the blood sugar. Multiple medications, also known as combination therapy is common in the treatment of diabetes! If one medication is not enough, you medical provider may give you two or three or more different types of pills. Insulin or other injected medications also may be prescribed. Or, depending on your medical condition, you may be treated only with insulin or injected medication therapy.
Many people with type 2 diabetes have elevated blood fats (high triglycerides and cholesterol) and blood pressure, so you may be given medications for these problems as well.
Maybe. Historically, 30% or more of people with type 2 diabetes required insulin therapy. However
there are many new drugs available that may delay or prevent the need for insulin therapy. It is
expected that fewer and fewer individuals will need insulin replacement to control their blood
sugars.
No. Taking insulin does not mean that you have type 1 diabetes. Your type of diabetes is determined by your genetics, not by the type of therapy.
Not necessarily. If you can lose weight, change your diet, increase your activity level, or change your medications you may be able to reduce or stop insulin therapy. Under certain circumstances, you may only need insulin temporarily – such as during pregnancy, acute illness, after surgery or when treated with drugs that increase their body’s resistance to the action of insulin (such as prednisone or steroids). Often the insulin therapy can be stopped after the event or stress is over.
Exercise is very beneficial in the management of type 2 diabetes. Always consult with your doctor about exercise guidelines, to exercise safely and reduce risks.
You may feel fine, but that is no guarantee that your blood sugar levels are in the target range. Remember, diabetic complications do not appear right away. And complications may develop even when the blood sugar is only slightly elevated. Regular blood sugar monitoring can help you keep your blood sugars in control and prevent serious damage to your eyes, kidneys and nerves. If your sugar levels are out of line, consult your doctor.
Yes. Type 2 diabetes is a genetic disease. The risk is highest when multiple family members have diabetes, and if the children also are overweight, sedentary and have the other risk factors for type 2 diabetes. Your child has a 10-15% chance of developing type 2 diabetes when you have type 2 diabetes. And if one identical twin has type 2 diabetes, there is a 75% likelihood of the other twin developing type 2 diabetes also.
Although we cannot change your genetic risk for developing type 2 diabetes, we do know that even modest exercise and weight loss can delay or prevent the development of type 2 diabetes. A landmark research study in the United States, the Diabetes Prevention Program (DPP) was completed in 2002 and showed that when people modified their risk factors for type 2 diabetes, they reduced their chance of developing the condition. Similar results have been shown in Finland.
In the DPP study, people with pre-diabetes were enrolled and assigned to 3 different treatments:
- Intensive lifestyle changes – exercise (30 minutes, 5 days a week), a healthy diet, and weight loss (loss of 7% of initial weight)
- The diabetes drug, Metformin
- An inactive placebo disguised as Metformin
The group that made lifestyle changes was 58% less likely to develop diabetes compared to the placebo group. And the group that took Metformin was 31% less likely to develop diabetes compared to the placebo group. In other words – lifestyle changes and Metformin therapy can delay or prevent the onset of type 2 diabetes. Lifestyle changes (weight loss, healthy diet and activity) are the most effective intervention.
There is not and ideal mix of carbohydrate, protein and fat that is right for everyone.Targets depend on your calorie goals, body weight, lipid profile, blood glucose control, activity levels, and personal preferences. A registered dietitian can help design a meal plan that is right for you.
The main lifestyle changes that lower blood pressure are weight loss and regular exercise. It’s also important to limit sodium and alcohol, and avoid smoking. Research from the National Heart Lung and Blood Institute (NHLBI) has shown that a diet low in total fat, saturated fat, and cholesterol, and rich in low fat dairy foods, fruits and vegetables, substantially lowers blood pressure.
B stands for Blood pressure control
C stands for Cholesterol.






